CANVax Briefs Series in CCDR
CANVax is collaborating with Canada Communicable Disease Report (CCDR) to publish short evidence-based briefs from our CANVax in Brief series throughout 2020.
These briefs will help inform, engage, and inspire readers by bringing attention to current and emerging issues in immunization, and by showcasing initiatives and activities from across Canada that aim to improve vaccine acceptance and uptake.
*Note: Previous versions of briefs originally published under the CANVax in Brief series are available upon request, contact us here.*
Articles:
- April 2021: Ethics check-up of public health immunization programs in Canada
- March 2021: Designing tailored interventions to address barriers to vaccination
- January 2021: Managing pain and fear: Playing your CARDs to improve the vaccination experience
- November/December 2020: Fake news and science denier attacks on vaccines. What can you do?
- October 2020: Benchmarking public health pain management practices during school immunizations
- September 2020: Vaccine injury compensation programs: Rationale and an overview of the Québec program
- July/August 2020: Considerations for mandatory childhood immunization programs
- June 2020: Managing immunization stress-related response: A contributor to sustaining trust in vaccines
- May 2020: Vaccine acceptance: How to build and maintain trust in immunization
- April 2020: Motivational interviewing: A powerful tool to address vaccine hesitancy
- February/March 2020: Optimizing communication material to address vaccine hesitancy
- January 2020: Promoting immunization resiliency in the digital information age
- January 2020: Editorial - A new resource to summarize evidence on immunization from the Canadian Vaccination Evidence Resource and Exchange Centre (CANVax)
Ethics check-up of public health immunization programs in Canada
Volume 47-4: COVID-19: A Year Later
Abstract
The World Health Organization (WHO) recognizes immunization as one of the most successful and effective public health interventions for saving lives. In developing a roadmap for prioritizing use of the coronavirus disease 2019 (COVID-19) vaccines in the context of limited supply, WHO highlighted the importance of a values (ethical principles) framework. Immunization does need to be subject to independent ethical scrutiny of vaccine research data, manufacturing practices, the legal and ethical assurance of informed consent, and also social justice issues with respect to program equity, including right to access. An ethics review of Australia’s immunization program was reported in 2012. This CANVax (Canadian Vaccination Evidence Resource and Exchange Centre) Brief offers an ethics review of immunization in Canada using the criteria utilized for Australia.
Designing tailored interventions to address barriers to vaccination
Volume 47-03, March 31, 2021: Influenza and Other Respiratory Viruses
Abstract
Despite efforts to promote vaccination and make vaccination services easily accessible, vaccination coverage rates remain below the target rate for many vaccines in various jurisdictions. The Tailoring Immunization Programmes (TIP) approach was developed by the World Health Organization Regional Office for Europe to support efforts of countries to achieve high and equitable vaccination uptake. In this Canadian Vaccination Evidence Resource and Exchange Centre (CANVax) series, we present key insights from the TIP planning framework to assist vaccine program planners, policy makers and vaccine providers to identify the interventions that will lead to increased vaccine uptake. The TIP is a phased approach that involves the following: 1) a clear diagnosis of the root cause of low vaccination; 2) an intervention based on this understanding; and 3) an evaluation of the implementation process and the impact of the interventions. At the provider-patient level, the approaches and insights of the TIP planning framework could inform vaccination consultation by emphasizing the importance of engaging with and listening to the patients and caregivers, and responding to their needs.
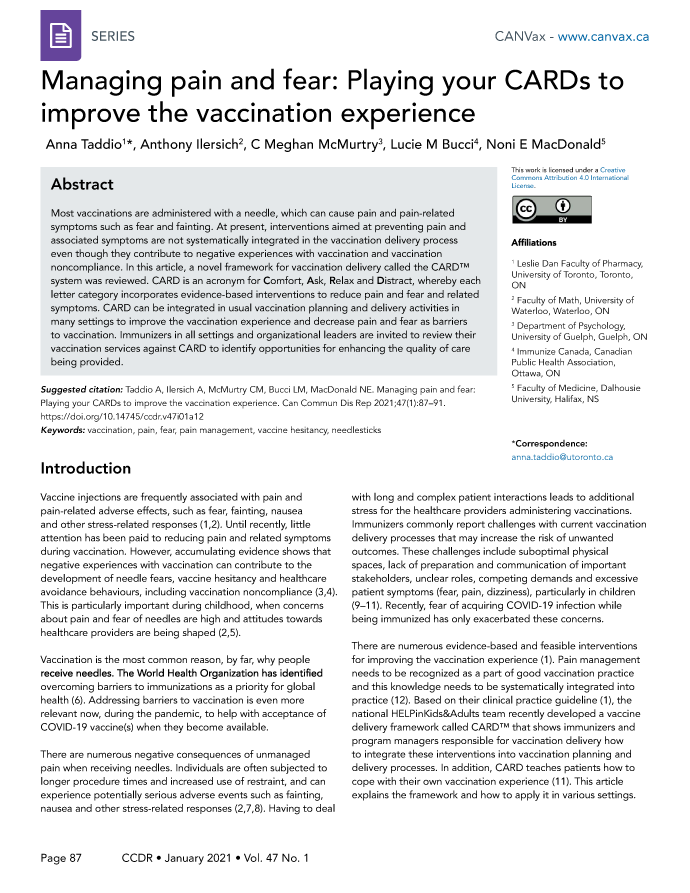
Managing pain and fear: Playing your CARDs to improve the vaccination experience
Volume 47-01, January 29, 2021: Foodborne and Animal Contact Disease Outbreaks
Abstract
Most vaccinations are administered with a needle, which can cause pain and pain-related symptoms such as fear and fainting. At present, interventions aimed at preventing pain and associated symptoms are not systematically integrated in the vaccination delivery process even though they contribute to negative experiences with vaccination and vaccination noncompliance. In this article, a novel framework for vaccination delivery called the CARD™ system was reviewed. CARD is an acronym for Comfort, Ask, Relax and Distract, whereby each letter category incorporates evidence-based interventions to reduce pain and fear and related symptoms. CARD can be integrated in usual vaccination planning and delivery activities in many settings to improve the vaccination experience and decrease pain and fear as barriers to vaccination. Immunizers in all settings and organizational leaders are invited to review their vaccination services against CARD to identify opportunities for enhancing the quality of care being provided.
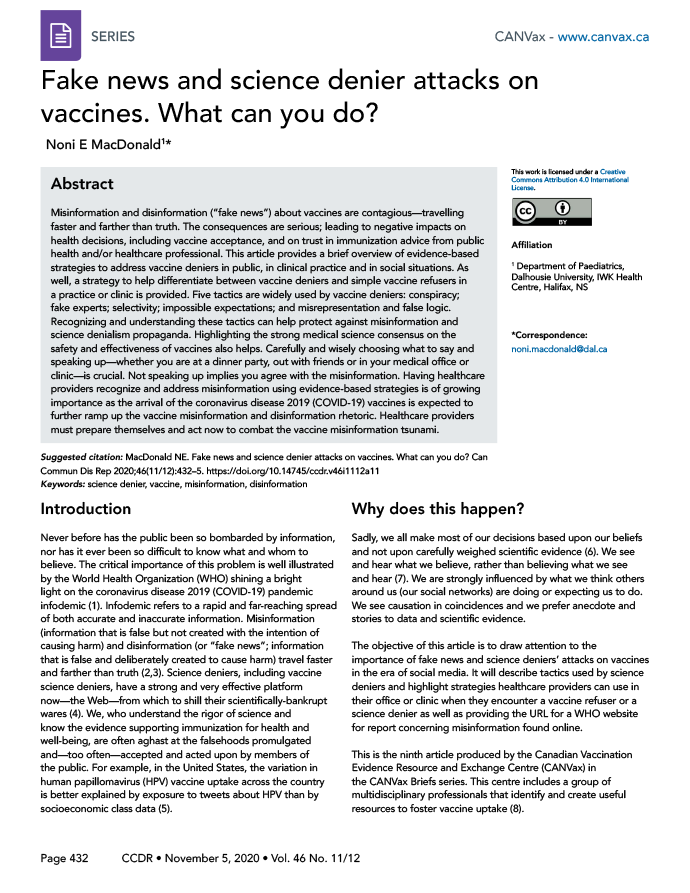
Fake news and science denier attacks on vaccines. What can you do?
Volume 46–11/12, November 5, 2020: Oral Health in Canada
Abstract
Misinformation and disinformation ("fake news") about vaccines are contagious—travelling faster and farther than truth. The consequences are serious; leading to negative impacts on health decisions, including vaccine acceptance, and on trust in immunization advice from public health and/or healthcare professional. This article provides a brief overview of evidence-based strategies to address vaccine deniers in public, in clinical practice and in social situations. As well, a strategy to help differentiate between vaccine deniers and simple vaccine refusers in a practice or clinic is provided. Five tactics are widely used by vaccine deniers: conspiracy; fake experts; selectivity; impossible expectations; and misrepresentation and false logic. Recognizing and understanding these tactics can help protect against misinformation and science denialism propaganda. Highlighting the strong medical science consensus on the safety and effectiveness of vaccines also helps. Carefully and wisely choosing what to say and speaking up—whether you are at a dinner party, out with friends or in your medical office or clinic—is crucial. Not speaking up implies you agree with the misinformation. Having healthcare providers recognize and address misinformation using evidence-based strategies is of growing importance as the arrival of the coronavirus disease 2019 (COVID-19) vaccines is expected to further ramp up the vaccine misinformation and disinformation rhetoric. Healthcare providers must prepare themselves and act now to combat the vaccine misinformation tsunami.
Benchmarking public health pain management practices during school immunizations
Volume 46–10, October 1, 2020: Laboratory Biosafety
Abstract
Background: Pain and fear during immunizations can affect children and their future behaviour toward immunization. These negative experiences can be amplified when children receive vaccines as part of school-based immunization programs, where parental or tutor supports are missing. In 2015, HELPinKIDS&ADULTS, a Canadian network of experts, published a clinical practice guideline (CPG) on the management of pain and fear during immunization. This guideline has been endorsed by international, national and provincial organizations. However, the level of integration and implementation of the CPG into local and community immunization programs such as school-based immunization clinics is unclear.
Methods: An investigation whether public health units in Ontario integrated and implemented the pain and fear interventions recommended by the CPG into school-based immunization policies and practices was concluded.
Results: The study shows that the majority of public health units do have pain and fear policies and procedures in place, but interventions are not integrated in a consistent and formal manner, leading to suboptimal uptake of interventions during immunizations at school.
Conclusion: For pain interventions to be applied with sufficient fidelity and in enough individuals to have a meaningful effect, organizational leaders need to create directives and procedures that support implementation in a systematic and accountable manner.
Vaccine injury compensation programs: Rationale and an overview of the Québec program
Volume 46 Issue 9, September 3, 2020: Force Health Protection
Abstract
Vaccines are among the safest therapeutic agents, and serious adverse events rarely occur. When they do occur, an individual may have to bear some or all of the costs associated with their injuries, seek compensation through litigation or, if available, seek compensation from a publicly-supported Vaccine Injury Compensation Program (VIC Programs). The VIC Programs are "no-fault" compensation schemes in which governments compensate individuals who are harmed by properly manufactured vaccines. There are ethical, legal and practical rationales to support these programs. Worldwide there are 19 countries that have implemented VIC Programs; in the majority of these countries, vaccines are not mandatory. They all have similar processes with respect to process, standard of proof and elements of compensation. In Canada, only the province of Québec has a VIC Program, which has been running successfully since 1985. Concerns with VIC Programs include cost, difficulties assessing causality and concern that such programs may undermine public trust in vaccines; but these concerns can be addressed, especially in high-income countries that can bear the costs and have the capacity to manage the program.
Considerations for mandatory childhood immunization programs
Volume 46–7/8, July 2, 2020: Mandatory childhood immunization programs
Abstract
Outbreaks of vaccine preventable diseases occur even in countries that have unrestricted and relatively equitable access to immunizations because vaccine uptake rates are lower than necessary for effective disease control. Vaccine hesitancy is seen in many countries, including Canada, and has led to enacting or strengthening legislation requiring mandatory childhood immunization in some provinces. Although mandatory immunization may seem to be the simplest solution to this issue, it is not always as effective as anticipated. Different countries/states/provinces/territories have used different strategies to encourage parents to fully immunize their children. Definition, scope, flexibility (such as exemptions for medical, religious and philosophical reasons) and framework factors (such as strictness of application and levels of enforcement of the mandate) vary widely between jurisdictions. Surprisingly, no marked differences were seen in vaccination rates between countries that recommended versus mandated them. Unintended consequences of mandatory immunization programs—both good (increased availability of data) and bad ("gaming" of the system and disproportionate impacts on families of lower socioeconomic status) have been reported. Addressing lower vaccine uptake rates is a complex problem that needs a multipronged, more nuanced and tailored approach.
Managing immunization stress-related response: A contributor to sustaining trust in vaccines
Volume 46–6, June 4, 2020: Artificial intelligence in public health
Abstract
Adverse events following immunizations (AEFI) are important to identify and manage effectively so as to sustain trust in vaccines and optimize health. The AEFI category related to “anxiety about the immunization” was considered problematic as it did not adequately capture the range of stress responses that can occur. The currently used term for this category, immunization stress-related responses (ISRR), is broader, including the full spectrum of signs and symptoms that can arise in response to stress. ISRR can include vasovagal reactions (fainting), hyperventilation and functional neurological symptoms (e.g. weakness, nonepileptic seizures). It is based on a biopsychosocial framework in which biological (e.g. age, sex), psychological (e.g. preparedness, previous experiences, anxiety) and social factors (e.g. response by others, social media) interact to create an individual’s stress response to the immunization process.
New guidance is available on prevention, early detection and management of ISRRs which is summarized in the article.
Vaccine acceptance: How to build and maintain trust in immunization
Volume 46–5, May 7, 2020: Nosocomial infection surveillance
Abstract
In Canada, over 80% of parents choose to vaccinate their children. Although this may appear positive, it is one of the lowest vaccination rates in the western world, and does not meet the 95% coverage rate needed to prevent outbreaks of vaccine-preventable diseases such as measles. A recent national immunization survey showed approximately 50% of parents are concerned about potential side-effects from vaccines, 25% believe that a vaccine can cause the disease it was meant to prevent, and 13% think alternative practices could eliminate the need for vaccines. In addition, vaccine hesitancy—defined by its determinants: confidence, complacency and convenience—is on rise. To address the complacency and trust (confidence) components of vaccine hesitancy, four best practices to optimize trust in vaccines and promote vaccine acceptance are presented. The first best practice is to understand the concerns; this is done at a population level via research and at individual level via motivational interviewing. The second best practice is to address these concerns by effectively presenting science-based information. This is done at a population level by communicating research and at an individual level by applying this research to the specific concerns, values and norms of the individual. Third, present immunization as a social norm, both in educational materials and in conversations. Finally, resilience is fostered by planning ahead (both at a population level and for individual practitioners) to manage events that can undermine trust and drive negative vaccine concerns, such as a new vaccine being added to the routine schedule or the emergence of an unexpected adverse event. Building and maintaining public trust in immunization takes time. Healthcare practitioners must keep in mind that while trust is a key element in vaccine acceptance, it is not the only element; convenience and access can also impact vaccine uptake. Nurturing trust is but one part of increasing vaccine acceptance and this brief will focus on strategies to build and nurture trust.
Motivational interviewing: A powerful tool to address vaccine hesitancy
Volume 46–4, April 2, 2020: Respiratory syncytial virus (RSV)
Abstract
According to the World Health Organization, vaccine hesitancy is among the top threats to global health and few effective strategies address this growing problem. In Canada, approximatively 20% of parents/caregivers are concerned about their children receiving vaccines. Trying to convince them by simply providing the facts about vaccination may backfire and make parents/caregivers even more hesitant. In this context, how can health care providers overcome the challenge of parental decision-making needs regarding vaccination of their children?
Motivational interviewing aims to support decision making by eliciting and strengthening a person’s motivation to change their behaviour based on their own arguments for change. This approach is based on three main components: the spirit to cultivate a culture of partnership and compassion; the processes to foster engagement in the relationship and focus the discussion on the target of change; and the skills that enable health care providers to understand and address the parent/caregiver’s real concerns.
With regard to immunization, the motivational interviewing approach aims to inform parents/caregivers about vaccinations, according to their specific needs and their individual level of knowledge, with respectful acceptance of their beliefs. The use of motivational interviewing calls for a respectful and empathetic discussion of vaccination and helps to build a strong relationship.
Numerous studies in Canada, including multicentre randomized controlled trials, have proven the effectiveness of the motivational interviewing approach. Since 2018, the PromoVac strategy, an educational intervention based on the motivational interviewing approach, has been implemented as a new practice of care in maternity wards across the province of Quebec through the Entretien Motivationnel en Maternité pour l’Immunisation des Enfants (EMMIE) program.
Optimizing communication material to address vaccine hesitancy
Volume 46–2/3, February 6, 2020: Public Health Network
Abstract
Vaccine hesitancy (the reluctance to accept recommended vaccines) is a complex issue that poses risk communication challenges for public health authorities and clinicians. Studies have shown that providing too much evidence on vaccine safety and efficacy to those who are vaccine-hesitant has done little to stem the growth of hesitancy-related beliefs and fears. The objective of this paper is to describe good practices in developing communication materials to address vaccine hesitancy.
An inventory of vaccination communication materials in Canada was assessed according to the Council of Canadian Academies Expert Panel on Health Product Risk Communication Evaluation (2015). Many of the current communication products could be improved to better align with evidence-based risk communication best practices. Five best practices were identified. First, identify target audience and establish trust. Second, provide both the risks and benefits of vaccination, as most people are looking for balanced information. Third, give the facts before addressing the myths. Fourth, use visual aids. Fifth, test communication material prior to launch.
Applying these best practices to current or future communication products will help vaccine providers (including physicians, nurse practitioners, pharmacists, public health professionals) to develop communication materials that are sensitive to the complex ways that people process and value information and thus more likely to optimize vaccine uptake in their communities.
Promoting immunization resiliency in the digital information age
Volume 46–1, January 2, 2020: Antimicrobial resistance (AMR)
Abstract
The avalanche of online information on immunization is having a major impact on the percentage of the population who choose to get vaccinated. Vaccine misinformation spreads widely with the interactive Web 2.0 and social media; this can bury science-based information. A plethora of immunization misinformation online is affecting trust in health care professionals and in public immunization programs. There are no simple solutions to this, but seven evidence-based strategies can help. First, listen to patients’ and parents’ concerns, and demonstrate responsiveness by adopting best immunization practices, such as pain mitigation. Second, recognize and alert others to anti-immunization tactics, namely, conspiracy theories, fake experts, selectivity, demands that vaccines be 100% safe and effective, misrepresentation and false logic. Third, avoid unproductive debates with those who have strongly held views, both in person and when using social media. Be respectful, stick to your key message, identify where to find useful information and exit. Fourth, consider establishing an attractive, easily searchable online presence that reflects the complex art of persuasion. Emphasize the benefits of vaccine, use reader-friendly graphics and highlight facts with stories to strengthen your case. Fifth, work with social media platform providers, not to stifle freedom of expression, but to help ensure that misinformation is not favoured in searches. Sixth, promote curriculum development in the schools to improve students’ understanding of the benefits and safety of immunization and to foster critical thinking skills. To do this, optimize the use of age-appropriate comics and interactive learning tools such as electronic games. Seventh, to shift the narrative in specific communities with low vaccination rates, work with community leaders to build tailored programs that foster trust and reflect local values.
Editorial - A new resource to summarize evidence on immunization from the Canadian Vaccination Evidence Resource and Exchange Centre (CANVax)
Volume 46–1, January 2, 2020: Antimicrobial resistance (AMR)
Abstract
Scientific progress around the development, use and best practices for communicating the benefits of vaccines is rapid, and keeping up-to-date with the substantial body of evidence on these topics is challenging. However, the increase in the number of vaccines and decline in vaccine-preventable illnesses has often focused public attention more on the risks of vaccines rather than the risks of the diseases. In Canada and elsewhere, an increasing number of parents are choosing to delay and/or refuse some or all vaccines for their children, leading to declining community protection against vaccine-preventable diseases and an increase in the number of outbreaks of vaccine-preventable diseases. Evidence suggests that the concept of vaccine hesitancy contributes to a deeper understanding of vaccination decisions by moving beyond the traditional binary of pro- or anti-vaccine attitudes to recognize a spectrum of beliefs and associated behaviours that occupies the space between the two poles. At a time of growing antimicrobial resistance to infections, protection conferred by vaccination is more important than ever.
The Canadian Vaccination Evidence Resource and Exchange Centre (CANVax) is an online curated database of resources to support immunization and promotional activities aimed at improving vaccine acceptance and uptake in Canada. It includes both the identification of accurate and reliable resources and the creation of new resources by a group of multidisciplinary professionals.
This issue of the Canada Communicable Disease Report (CCDR) includes the first of a series of “CANVax Briefs” that have been developed by experts after conducting scoping reviews and environmental scans and assessing the most rigorous evidence. The aim of the CANVax Briefs is to bring attention to current and emerging issues by providing short summaries of the recent best available evidence to assist frontline public health and clinical care professionals in optimizing the immunization rate in Canada. CANVax Briefs will be published in CCDR throughout 2020.